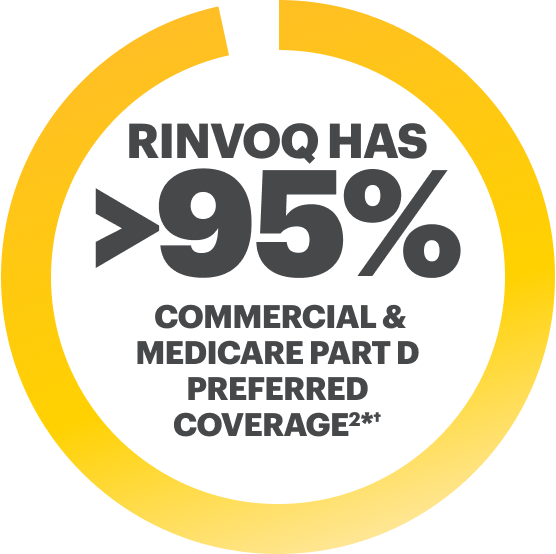
National Commercial and Medicare Part D formulary coverage under the pharmacy benefit as of May 2025 in AD.2
COMMITTED
TO EXCEPTIONAL ACCESS
Help your appropriate patients get started on RINVOQ Complete by downloading these important access forms.
Enroll your patients in
Offers comprehensive access and reimbursement support, education, and financial assistance.

Affordability
Eligible, commercially insured patients may pay as little as $0 per month on their RINVOQ prescription and can be reimbursed for the out-of-pocket costs of related lab tests and monitoring.‡

Bridging Patients
No charge for eligible patients experiencing initial insurance denial for up to 24 months.§

Access Support
Your Field Reimbursement Manager (FRM) is your primary contact to provide education and support related to access and reimbursement questions and activities. FRMs have expertise in Complete access resources and can help build confidence in navigating an ever-changing access landscape.

1-to-1 Patient Support
Your enrolled patients can receive 1-to-1 support from their dedicated Nurse Ambassador|| and Insurance Specialists to help them explore savings options, navigate changes in their health insurance coverage, understand their condition, and learn how to take and store RINVOQ as prescribed.
||Nurse Ambassadors are provided by AbbVie and do not provide medical advice or work under the direction of the prescribing health care professional (HCP). They are trained to direct patients to speak with their HCP about any treatment-related questions, including further referrals.
Check the Formulary Status for RINVOQ in Your Area
Formulary Zipcode
Choose Indication
Formulary Status Results
- Plan Name
- Plan Type
- Status
Results ends here
- Plan Name
- Plan Type
- Status
Results ends here
Preferred means RINVOQ is on a preferred tier or otherwise has preferred status on the plan’s formulary.

Additional resources are available to support your patients in accessing and receiving treatment with RINVOQ
*RINVOQ is on a preferred tier or otherwise has preferred status on the plan’s formulary.
†Coverage requirements and benefit designs vary by payer and may change over time. Please consult with payers directly for the most current reimbursement policies.
‡Eligibility: Available to patients with commercial insurance coverage for RINVOQ who meet eligibility criteria. This co-pay assistance program is not available to patients receiving prescription reimbursement under any federal, state, or government-funded insurance programs (for example, Medicare [including Part D], Medicare Advantage, Medigap, Medicaid, TRICARE, Department of Defense, or Veterans Affairs programs) or where prohibited by law. Offer subject to change or termination without notice. Restrictions, including monthly maximums, may apply. This is not health insurance. For full Terms and Conditions, visit RINVOQSavingsCard.com or call 1.800.2RINVOQ for additional information. To learn about AbbVie’s privacy practices and your privacy choices, visit https://privacy.abbvie
§Eligibility criteria: Available to patients aged 63 or younger with commercial insurance coverage. Patients must have a valid prescription for RINVOQ for an FDA approved indication and a denial of insurance coverage based on a prior authorization request on file along with a confirmation of appeal. Continued eligibility for the program requires the submission of an appeal of the coverage denial every 180 days. Program provides for RINVOQ at no charge to patients for up to two years or until they receive insurance coverage approval, whichever occurs earlier, and is not contingent on purchase requirements of any kind. Program is not available to patients whose medications are reimbursed in whole or in part by Medicare, Medicaid, TRICARE, or any other federal or state program. Offer subject to change or discontinuance without notice. This is not health insurance and program does not guarantee insurance coverage. No claims for payment may be submitted to any third party for product dispensed by program. Limitations may apply.



